Weight Loss: Insulin, Blood Sugar, Stress, Sleep and Cortisol
Written by Dr Arien van der Merwe
The blood sugar craze
With the epidemic of diabetes and metabolic syndrome plaguing the Western world, blood sugar and insulin have gotten their fair share of media attention. Blood sugar balance is a major principle of virtually every diet book from The Zone to The Atkins Diet. And with good reason: imbalanced blood sugar (glucose) levels are the root cause of many health issues, including being overweight, obesity, premature or accelerated ageing, and chronic inflammation.
Practical considerations
In my practice, I see people with blood sugar imbalances every day. Not all of them are obese, or even overweight! Some are health conscious. They do not eat takeaways, sweets, ‘slap’ chips, doughnuts, or laze around in front of the TV. Some eat well, exercise regularly, have normal body composition and take supplements, but still don’t feel well, with low energy, fatigue and even depression. They, too, are coming in with blood sugar issues of which they weren’t even aware!
Let’s consider two paths
When talking about blood sugar balance, there are two main possibilities:
1. Insulin resistance
Categorised by two things: chronically elevated blood sugar levels, and subsequent elevated insulin levels to help deal with the blood sugar, with muscle and fat cells’ receptors becoming resistant to insulin, therefore less glucose is able to enter cells for optimal use as fuel for cell function.
2. Hypoglycemia or low blood sugar
More accurately described as fluctuations in blood sugar: sometimes high and sometimes low.
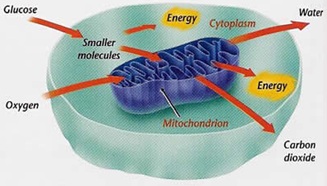
Both paths have insulin surges. While each of these have their separate metabolic effects, both will cause problems in the functioning of the mitochondria,or power generators of the cell, because there isn’t a constant, balancedsupply of blood sugar available for consistent ATP (energy producing molecule) production.
Insulin resistance
With insulin resistance, glucose cannot effectively enter into the cell. If insulin doesn’t bind to its receptor on the cell membrane, the glucose channels cannot open, and insufficient quantities of glucose enter the cell. This chronically elevated insulin levels create more and more dysfunctional insulin receptor sites on the cell membrane.
Because blood sugar is not adequately entering the cells, it stays in general circulation rather than being utilised for energy inside the cell. As a result, the body must produce higher levels of insulin to try to remove glucose from t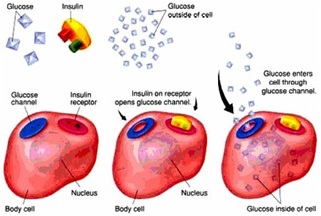 he blood stream, which causes even greater metabolic dysfunction. The increased blood sugar, also leads to insulin’s second function, fat synthesis (i.e. storing the perceived excess glucose as fat – storage for later use!). In the meantime, the cells are starved, claiming for more food for energy and fuel! A vicious circle – we cannot fight the primary drive of hunger for survival that arises from cells starving for lack of fuel!
he blood stream, which causes even greater metabolic dysfunction. The increased blood sugar, also leads to insulin’s second function, fat synthesis (i.e. storing the perceived excess glucose as fat – storage for later use!). In the meantime, the cells are starved, claiming for more food for energy and fuel! A vicious circle – we cannot fight the primary drive of hunger for survival that arises from cells starving for lack of fuel!
Characteristic symptoms of insulin resistance include: fatigue after meals, craving for sweets that doesn’t go away when sweets are eaten, increased thirst, and frequent urination.
Elevated insulin is also a major cause of ageing and chronic inflammation!
Hypoglycemia
Clinically, hypoglycemia can be viewed as fluctuations in blood sugar. People with hypoglycemia can experience symptoms such as lightheadedness, irritability, shakiness, nausea, irritability, poor concentration and fatigue between meals, which is often relieved after eating. These symptoms are stress symptoms generated by the body as a call for fuel, that is, glucose. The stress symptoms also lead to an increase in cortisol levels – the long term stress hormone.
Individuals with th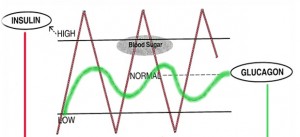 is pattern and periods of low blood sugar will have surges of insulin, rather than chronically elevated levels. Normally, the body should respond to low blood sugar by producing cortisol to increase blood sugar levels. However, in this case, periodically hypoglycemic people usually have low adrenal function and rely on adrenaline (to break down glucose stores – glycogen) to elevate blood sugar between meals, which causes the shakiness and lightheadedness between meals. Symptoms are usually relieved after eating, because meals provide a source of glucose, the body’s primary source of fuel.
is pattern and periods of low blood sugar will have surges of insulin, rather than chronically elevated levels. Normally, the body should respond to low blood sugar by producing cortisol to increase blood sugar levels. However, in this case, periodically hypoglycemic people usually have low adrenal function and rely on adrenaline (to break down glucose stores – glycogen) to elevate blood sugar between meals, which causes the shakiness and lightheadedness between meals. Symptoms are usually relieved after eating, because meals provide a source of glucose, the body’s primary source of fuel.
Often though, people with low blood sugar will eat too much high glycemic starch (chocolates, sugary food, cookies) or even too much healthy food, because of extreme hunger, and their blood glucose levels shoot up, causing too much insulin released by the pancreas, clearing away the glucose too efficiently, and then leading to even worse symptoms than before they ate. This is called ‘dumping’. The best is to eat small, healthy snacks in between healthy meals: a handful of nuts, or a slice of low GI, whole wheat or rye, bread, or yoghurt, some dried fruit, 2 provitas or other whole grain biscuits.
Because their bodies rely on adrenaline to elevate blood sugar, people with hypoglycemia can have insulin surges between meals.
| Hypoglycemic tendencies | Insulin resistant tendencies |
| Feels better after meals | Feels tired after meals |
| Sugar craving before meals | Sugar craving after meals |
| May have difficulty asleep at night | May have difficulty getting to sleep at night |
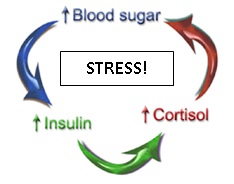
The cycle commonly found in people, with, or without, obesity, or being overweight: low blood sugar leading to symptoms of distress, then eating too much even of healthy food (often becoming obsessed with snacking), with surges in blood sugar levels, leading to increased insulin levels, leading to increased cortisol levels, leading to higher blood sugar levels, feeling more distressed, and so on: truly a vicious circle!
Another way this cycle can be activated is via cortisol to start with. Cortisol is the long term stress hormone. Anything that elevates cortisol (i.e. high stress levels, infection, food allergies, inflammation, etc.) will also elevate blood sugar (to provide fuel for the classic stress reaction: fight or flight) and therefore insulin levels. In other words, you could have a perfect diet and exercise program, but if you have elevated cortisol levels, you may also be increasing your blood sugar from the inside. Cortisol is responsible for keeping the pantry filled to survive the lean years – the pantry being your abdomen!
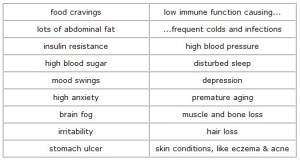
Symptoms of high cortisol levels, mostly due to being in an inner state of high stress (distress):
Symptoms of chronically elevated insulin levels
Insulin is necessary for life. Without it, we cannot live. But as with most hormones, insulin should be balanced. In excess, elevated insulin levels have many negative effects on the body.
Solutions
-
Thorough evaluation – the first step.
You cannot manage what you do not know of! Go for a thorough health screening that includes lipid profile, thyroid, liver and kidney function, as well a medical assessment of blood pressure, waist circumference and body composition. Have your fasting (early morning before breakfast) blood glucose and insulin levels assessed, as well as cortisol levels before 10h00. Complete a comprehensive health and stress assessment, that includes the self test for potential neurotransmitter (informational peptides)deficiencies that can be easily corrected with natural remedies that restore balance and function to all four main neurotransmitters: dopamine, serotonin, GABA (gamma amino butyric acid) and acetylcholine.
| Hypoglycemic | Insulin resistance- also linked to metabolic syndrome |
| Fasting blood sugar below 4.5mmol/L |
|
These are general guidelines and risk identification values.It is important to consult a qualified medical professional, specialising in natural and integrative medicine, for an accurate diagnosis and management of health risks through coaching and discussions.
-
Embark on a journey into healing.
healthy eating and moderate, enjoyable exercise, regular contact with nature, meditation, affirmative or positive prayer to reconnect on a daily basis to your true, authentic self and re-learning how to play, have fun and enjoy life, not looking for, but finding, ‘sweetness in life’ – the mental emotional underlying issue in insulin resistance and metabolic syndrome. After all, joy, playfulness, having fun and experiencing inner peace, while being fully and vibrantly alive, are all aspects of our ultimate purpose as human beings (rather than human doings) in this lifetime!
-
Dietary guidelines (only a summary).
The rationale behind ahigher protein-based diet, with adequate levels of vegetables, low GI fruit, low quantities of low GI carbohydrates, healthy fat and fibre,is that it should not raise your blood sugar levels too high, thereby keeping insulin levels within normal boundaries. If insulin levels still rise too much, the macronutrient (protein, fat, carbohydrates) ratio was out of balance, the meal too big, or you might have a sensitivity to the food that causes a stress response and elevates blood sugar.
-
Proper breathing practice.
Blood sugar imbalances and elevated insulin levels have negative impacts on many physiological systems in the body. On a fundamental level, if adequate glucose cannot enter a cell, the mitochondria (the cell’s power generators) will not be able to produce optimal amounts of ATP, the energy molecules, to run the cells, organs and systems of the body, and we will not be optimally healthy, much less have the body we desire. We’ll feel tired, or even extremely fatigued, low in energy, unable to enjoy our lives.
We need oxygen to live. Together with blood glucose or sugar, oxygen is one of the two fuel sources for one of the most important components of your cell: the mitochondria or power generators. Without oxygen and glucose, it is impossible for your cells to work at their full capacity or for you to be optimally healthy, happy and full of energy. Lack or below optimal quantities of either or both, will manifest in hormonal, thyroid, cardiovascular, neurological, or weight release health challenges.
-
Sleep restoration
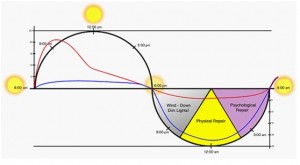
through following your natural sleep-wake rhythm or circadian cycle is another of the most important ways of keeping cortisol levels balanced during the day.
Our body, including our mind, brain and emotions, operate on a biological clock set to daily cycles, known as circadian rhythms. We normally feel more alert during the daylight hours and less alert at night, a fact of life even for people who have worked nights for a very long time.
Cortisol levels start decreasing after about 4 hours of deep sleep in quiet and darkness, reaching its lowest levels after about 6-7 hours, to slowly rise and waking us up naturally after 7-8 hours of sleep. On the other hand, melatonin (the rest, recovery and replenishing hormone secreted by the pineal gland) start rising in the same sequence, to reach its zenith after 6-7 hours of deep sleep in quiet and darkness, slowly decreasing so that we wake up naturally after 7-8 hours of restful sleep, ready to face our day. Deep relaxation or meditation any time of the day, for one hour, is equivalent to 3 hours of deep sleep.
Sleep is critical to health, wellness& longevity and a vital physical need. We require sleep for survival just as we need food, water and oxygen.
The biggest obstacle to falling and staying asleep is that we fail to relax before trying to fall asleep:
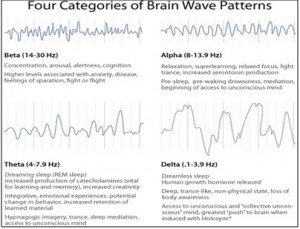
When awake and alert, our brain waves are predominantly in the beta brain wave state, with fast, sharp waves. These waves are easily distinguishable on an electro encephalogram (EEG). The more alert, stressed or worried we are, the higher and faster these beta waves become. High states of beta rhythm are also linked to all our physical ailments and chronic diseases such as high blood pressure, anxiety, depression, heart disease, insulin resistance, metabolic syndrome, diabetes, etc.
As we prepare for sleep, brain waves slow down to alpha rhythm, a state of relaxed awareness. We gradually loose awareness of time and space, feeling more and more relaxed and at peace. We then slip into sleep which is identified by theta brain waves of an even slower frequency. This is also the brain wave state where we dream. Ultimately we go into delta sleep, the deep dreamless sleep where true restoration and recovery of our bodies and minds take place. We move through about 6 cycles of these brain wave states throughout the night. Sleeping tablets prevent the normal cycles of sleep. That is the reason people feel groggy and not rested after taking sleeping pills.
If the brain remains too alert, we cannot relax and fall asleep. A sleep ritual can help prepare you for sleep. Calm down before you go to sleep, with a sleep inducing drink (hot milk with some cinnamon and honey), the firm intention to sleep well, a warm bath, adding some aromatherapy oils of lavender or chamomile to the water; doing stretching exercises and a meditation or progressive muscle relaxation before you try to fall asleep, or listen to guided visualisations on a CD next to your bed.
-
Learn to relax:
Sit in a comfortable chair, or lie on your back. Breathe in deeply through your nose on a slow count of three. Push your stomach out as you breathe in. Hold it for a count of three. Breathe out through your mouth on a slow count of five or six. Repeat a few times until you feel relaxed. Feel your pulse rate by placing your fingers gently on your wrist below the thumb. When you’re stressed, it’s fast. Do the slow breathing for a while, and feel how your pulse rate slows down – this is a way your body will show you if you’re relaxed or not.
Deep relaxation, being the opposite of the fight-flight, cold-hunger survival fear response, enhances the health of your heart and lungs, balances the endocrine and nervous system, and improves mental clarity.
Imagine your thoughts being the waves on the surface of the ocean. They go up and down as the mood, your feelings, emotions and your memory dictate. The deeper ocean is quiet, still and peaceful. This is the part you can access any time of the day or night through meditation, visualisation, deep breathing and prayer. This is the secret to health, happiness and a long life!
Comparing brain patterns before and after relaxation:
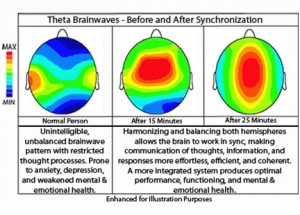 The purpose of relaxation training is therefore to optimise left brain function in beta rhythm while awake, without beta waves becoming too high (therefore too stressed), so that adrenalin, noradrenalin and cortisol levels are optimal. Then, during regular periods during the day and before sleep, to optimise right brain function, relaxing into alpha, theta and delta rhythm and ultimately integration of the whole brain for development of all our abilities as human beings to live a fulfilled life of joy, health and happiness, peace, being on purpose as joyful co-creators of heaven on earth, our birthright as human beings. The more we practice this, the more we’ll be able to switch between these natural states at will whenever we choose to do so.
The purpose of relaxation training is therefore to optimise left brain function in beta rhythm while awake, without beta waves becoming too high (therefore too stressed), so that adrenalin, noradrenalin and cortisol levels are optimal. Then, during regular periods during the day and before sleep, to optimise right brain function, relaxing into alpha, theta and delta rhythm and ultimately integration of the whole brain for development of all our abilities as human beings to live a fulfilled life of joy, health and happiness, peace, being on purpose as joyful co-creators of heaven on earth, our birthright as human beings. The more we practice this, the more we’ll be able to switch between these natural states at will whenever we choose to do so.
Self talk and the stress connection
Adrenalin (the hormone that increases in response to excess levels of insulin in the body) is a stress-response chemical, released under conditions of emotional upset. Glucocorticoids (such as cortisol) are also stress-response chemicals in some women, based on the cold and hunger primary instinctual drive (therefore unconscious), for which fat is the best protection! These hormones are also responsible for increased storing of abdominal fat and raising blood glucose levels. One study demonstrated that persons with elevated levels of serum cortisol (caused by chronic stress) developed abdominal obesity, insulin resistance and lipid abnormalities.
When I see patients at the Weight Control Clinic, the first words most say, are: I’m fat, I hate my body, I have to get rid of this ugly fat – or other words in this vein. This kind of self talk creates a feeling of cold and hunger inside the body-mind. This is a primary instinctual drive for survival (the other being the fight-flight-freeze response). It is a powerful drive that no will power or conscious control can ever subdue. Your body wants to save you from danger (your own thoughts and feelings!) and the best protection: fat, especially around the abdomen. Guilt is another primary cause for cold and hunger response. The only way to manage this, is to become aware of your self talk, finding the original cause of these feelings (often with the help of spiritual healing to access the deeply buried, subconscious beliefs) and gradually changing this to feeling love, gratitude and acceptance for your body trying to protect you. That’s when thebody will release the fat and it simply starts melting away. You feel better, you eat healthier, you move your body, from a deep inner soul urge to care for and protect your precious body. Then weight problems become a thing of the past.
Clearly, management of stress factors is a critical component to addressing the symptoms of metabolic syndrome.Shift work, sleep deprivation and bright light exposure at night also relate to increased body mass leading to metabolic syndrome. Recently, vitamin D deficiency was linked to the risk of cardiovascular disease and low vitamin D was strongly associated with overweight, obesity and metabolic syndrome.
The solution:
An integrative medicine approach, that includes a health screening with a comprehensive stress and depression assessment, followed by a medically assisted weight release program with motivation and ongoing support from health care practitioners, fun fitness, nutriceuticals (e.g. specific vitamins, herbs, amino acids and minerals), mental-emotional and nutritional guidance, advice on combating carbohydrate addiction and a support network that will assist in changing unhealthy lifestyle choices and behaviour to healthy and sustainable lifestyle choices.
Of the utmost importance:
Addressing subconscious emotional blockages from stressful or traumatic events in the recent past, or long forgotten memories, that play an important role as causal factor in the specific symptoms of metabolic syndrome. In short, struggling with metabolic syndrome is not due to lack of will power – there are more factors involved in this health challenge found in more than one third of the general population!
Definition of metabolic syndrome
A unified definition was finalised after a collaboration between the International Diabetes Federation, American Heart Association/National Heart, Lung and Blood Institute, the World Heart Federation, International Atherosclerosis Society and the International Association for the Study of Obesity. This new published definition involves the following factors:
- Increased waist circumference: Population – specific and country specific cut-off points to be used. Usually abdominal circumference more than 102 cm in men, and more than 88 cm in women
- Increased triglycerides (or drug treatment for it):1.7mmol/1 or above.
- Reduced HDL (or drug treatment for it) : < 1.0 mmol/l for men; < 1.3 mmol/l for women.
- Elevated blood pressure (or antihypertensive drugs used): 130 mmHg systolic; 85mmHg diastolic or above.
- Increased fasting glucose (drug treatment for increased glucose) >5.5 mmol/1.
Integrative approach to manage the battle of the bulge and the insulin connection:
- Behaviour modification, including a change in eating patterns with a specific kick start diet to lower insulin levels, then adjusting to a healthy diet withspecific seasonally available vegetables and fruit, nuts, seeds, low glycemic index carbohydrates, healthy fats and portion controlled protein from fish, poultry and lean meat, with increased intake of fibre rich food.
- Regular, gentle, enjoyable exercise matched to the individual fitness level. Cells with low glucose levels due to insulin resistance, are starving, and you will simply not have enough intracellular fuel to do strenuous or even moderate, exercise.
- The use of specific nutriceuticals and nutritional factors specifically designed for managing metabolic syndrome and addressing insulin resistance: e.g. beta-glucan from oats, antioxidants from berries, alpha-lipoic acid (ALA), omega 3 fatty acids, chromium, biotin, vanadium, phaseolamin (Phase 2) and the vitamins that will reduce blood homocysteine levels, such as folic acid and vitamins E and B12.
- Gymnema sylvestre, Hoodia gordonii as P57 extract, fenugreek and cinnamon are herbs that increase insulin receptor sensitivity and glucose metabolism.
- Reduction in blood pressure will be a result of weight control and lifestyle changes.
- The oxidative stress and advanced glycation end products may be reduced by bioflavonoids, proanthocyanidins, alpha lipoic acid and other antioxidants. High dosages of B-complex vitamins improve glucose metabolism.